Medical note: This guide is educational and not a substitute for personal medical advice. Always consult your clinician—especially if you have chronic kidney disease, heart failure, diabetes, swallowing difficulties, or take blood thinners.
Why Nutrition Matters for Healthy Aging
Nutrition shapes strength, balance, wound healing, and independence. In this clinician-vetted guide to nutrition for elderly adults, you’ll get practical, safe steps—and quick links to focused deep dives on protein, hydration, fiber, bone health, vitamin B12, and medication organization. Use this as your hub and explore each topic chapter when you’re ready.
For a foundational overview, see the National Institute on Aging’s Healthy Eating guidance.
At-a-Glance Checklist
- Prioritize protein at each meal (aim ~25–35 g per meal).
- Hydrate consistently (≈ 1.5–2 L/day unless restricted).
- Get 25–30 g fiber/day from food first; add a supplement only if needed.
- Support bones with calcium + vitamin D; screen for B12 deficiency.
- Use a pill organizer or automatic dispenser to reduce missed or double doses.
Related safety reads:
Understanding Fall Risks in Seniors and How to Prevent Them | Best Walkers & Rollators for Seniors (2025 Guide) | Best Shower Seat for Elderly (2025 Guide to Safe Bathing Chairs)

Why Nutrition for Elderly Adults Drives Mobility
After 60, muscle naturally declines (sarcopenia), bone density drops, thirst cues dull, and medication lists grow. A solid plan for nutrition for elderly adults protects strength and balance, fuels rehab, supports wound healing, prevents constipation and dehydration, and keeps thinking sharp.
Think of nutrition as your foundation for mobility—the stronger that base, the longer you stay active and independent.
Red Flags: When to Call Your Clinician
Unintentional weight loss, poor appetite, frequent falls, new confusion, persistent constipation or diarrhea, swallowing trouble, leg swelling, or wounds that aren’t healing are all reasons to call your clinician. Ask whether labs like CBC, CMP, vitamin D, B12, iron studies, and prealbumin are appropriate, and review medications that may affect appetite, hydration, or bowel function.
Key Nutrients for Healthy Aging
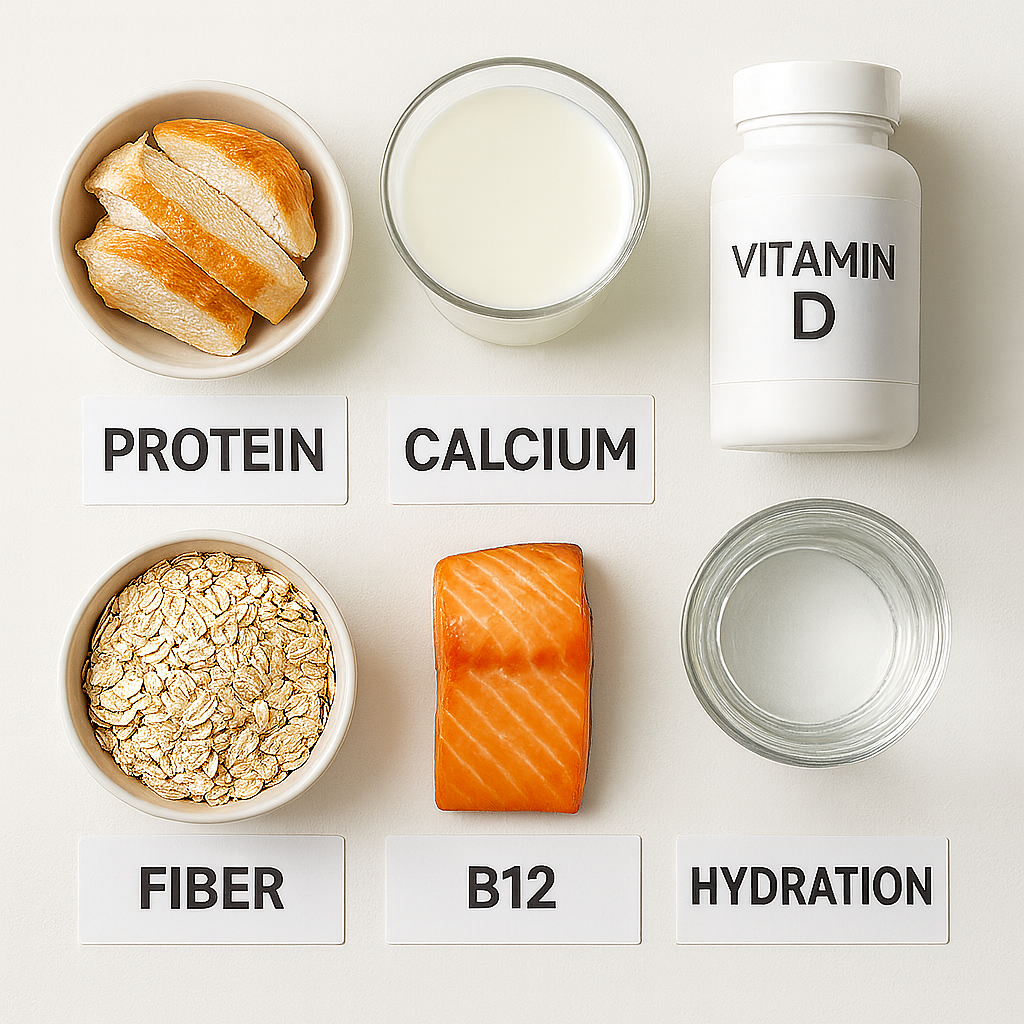
Protein
Aim ~1.0–1.2 g/kg/day, increasing to 1.2–1.5 g/kg/day during illness or rehab with clinician guidance. Evenly space protein (25–35 g per meal) to stimulate muscle synthesis.
Best sources: eggs, Greek yogurt, poultry, fish, tofu, beans + whole grains.
Calcium & Vitamin D
Calcium ≈ 1,200 mg/day (women 51+, men 71+) and vitamin D ≈ 800–1,000 IU/day keep bones strong. Combine with weight-bearing exercise for best results.
Fiber
Target 25–30 g/day from fruits, vegetables, beans, oats, and whole grains. Adequate fiber helps bowel regularity, heart health, and blood-sugar control.
Vitamin B12
B12 absorption drops with age and certain medications. Include seafood, dairy, and fortified foods; vegetarians/vegans may need supplements.
Hydration & Electrolytes
Drink 1.5–2 L/day unless restricted. Soups, fruit, and yogurt contribute to fluid intake. Choose low-sugar electrolyte options when needed.
Macronutrients & Micronutrients in Aging

As metabolism naturally slows after 60, every bite matters more. Choosing nutrient-dense foods—those high in vitamins, minerals, and protein for their calorie content—helps maintain muscle and energy while controlling weight and blood sugar.
Carbohydrates
Favor complex carbs from whole grains, fruits, and vegetables rather than refined starches. Fiber-rich carbs keep digestion regular and steady blood glucose, reducing risk of diabetes progression. Oats, quinoa, lentils, and sweet potatoes are excellent staples.
Fats
Healthy fats aid absorption of vitamins A, D, E, and K and support brain health. Prioritize omega-3-rich sources like salmon, sardines, walnuts, chia, and flaxseed. Use olive or avocado oil for cooking; limit deep-fried or heavily processed snacks.
Sodium & Flavor Balance
Older adults often lose taste sensitivity, tempting higher salt use—but too much sodium raises blood pressure and fluid retention. Enhance flavor with herbs, garlic, citrus, or vinegars instead of extra salt.
Micronutrients That Matter
Key micronutrients for mobility and cognition include vitamin D, calcium, magnesium, zinc, and B-vitamins. Because absorption can decline with age or medication use, food variety becomes your best defense against deficiency.
For a deeper dive on micronutrient safety and sources, visit the NIH Office of Dietary Supplements.
Protein for Strength & Balance
Most older adults do well around 1.0–1.2 g protein/kg/day; during illness, rehab, or wound healing, 1.2–1.5 g/kg/day may be required with supervision. Distribute protein evenly across meals to support lean mass and recovery.
Good choices: eggs, Greek yogurt, cottage cheese, poultry, fish, tofu/tempeh, beans + whole grains, and protein-fortified dairy.
Use caution: advanced CKD not on dialysis, severe liver disease—get individualized targets.
See: Protein for Elderly: Essential Daily Requirements & Proven Tips for Seniors (2025 Guide)
Compare supplements: Best Protein Powders for Seniors
Use the simple calculator below to estimate your personal daily protein target, then check the full guide for detailed examples.
Quick Protein Target Calculator
Estimate your daily protein needs for healthy aging and recovery.
Hydration & Electrolytes

Daily target ≈ 1.5–2 L, adjusted for size, climate, diuretics, and clinical limits.
Tips: keep a marked bottle nearby, sip with every medication, and include water-rich foods.
Warning signs: fatigue, dizziness, dark urine, constipation.
Electrolytes: choose low-sugar options during heat, illness, or diuretic use; avoid ultra-sweet or high-caffeine drinks.
Always consult your clinician first if you have heart failure or CKD.
Deep dives: Hydration Tips for Seniors | Best Electrolyte Drinks/Packets for Seniors (Coming soon)
Learn more: MedlinePlus: Dehydration
Digestive Health: Fiber & Constipation
Goal = 25–30 g fiber/day + adequate fluid. Increase slowly (~ +5 g/week) to avoid gas. Mix soluble (oats, beans, psyllium) for soft stools and cholesterol control with insoluble (vegetables, wheat bran) for regularity.
Food-first moves: oatmeal + berries; lentil soup; whole-grain toast; chia or flax; veggies at lunch and dinner.
Supplements: psyllium is well-tolerated and heart-healthy; methylcellulose works if gas is an issue. Always increase water.
Deep dives: Constipation in Seniors: A Food-First Plan (Coming soon) | Vitamin D & Calcium Basics for Seniors (Coming soon)
Consumer overview: MedlinePlus: Dietary Fiber
Bone Health: Calcium, Vitamin D & Movement
Bone strength depends on calcium + vitamin D + protein + exercise. Typical intakes: calcium ≈ 1,200 mg/day; vitamin D ≈ 800–1,000 IU/day (adjust by lab values).
See NIH Office of Dietary Supplements fact sheets: Vitamin D and Calcium.
Deep dive: Vitamin D & Calcium Basics for Seniors (Coming soon)
Brain & Nerve Support: Vitamin B12

B12 deficiency is common with age, especially with acid-suppressing meds or metformin. Symptoms: fatigue, memory issues, neuropathy. Include seafood, eggs, dairy, and fortified foods; vegans require supplementation.
Deep dive: Vitamin B12 in Older Adults (Coming soon) | NIH ODS Vitamin B12 Fact Sheet
Medication Timing, Interactions & Organization
Calcium, iron, thyroid meds, and some antibiotics compete for absorption—spacing doses can matter. Warfarin requires consistent vitamin K intake.
A pill organizer or automatic dispenser reduces missed doses and double-dosing, especially when multiple caregivers assist.
Deep dive: Best Pill Organizers & Automatic Dispensers (Coming soon)
Supplements & Safety

Food first whenever possible. Supplements fill gaps but can interact with medications or overlap in dose.
- Protein powders help when appetite is low but should not replace meals.
- Calcium and vitamin D may be needed if dietary intake is low.
- Multivitamins are rarely necessary unless diet is limited.
- B12 is safe and important if you are deficient or vegan.
Always review your supplement list with a clinician or pharmacist at least twice per year.
Simple 7-Day Meal Framework (Mix & Match)
Use this to hit protein, fiber, and hydration goals without complex cooking. Adjust texture for chewing or swallowing issues (involve a speech-language pathologist if needed).
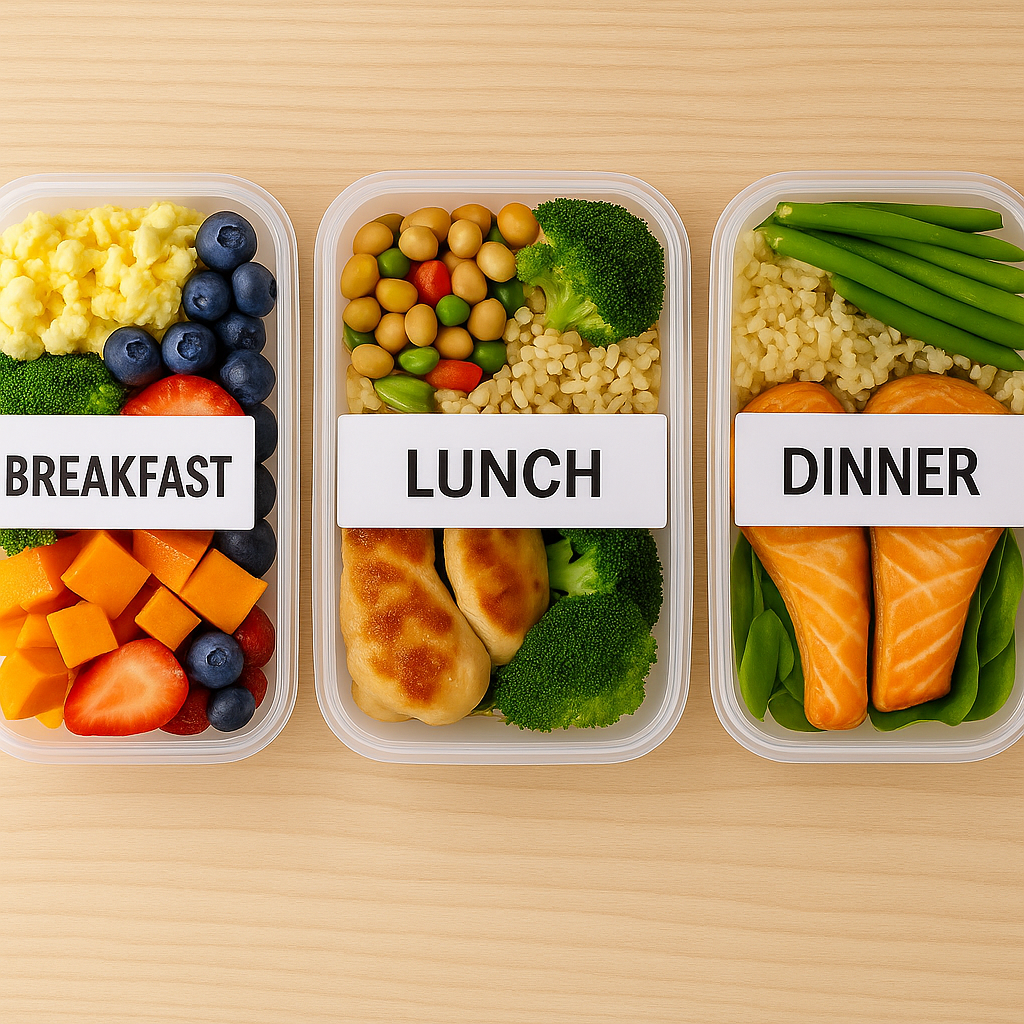
Breakfast rotation: Greek yogurt + berries + chia; veggie omelet + whole-grain toast; oatmeal + protein powder; cottage cheese + pineapple + walnuts.
Lunch rotation: Lentil or chicken soup + side salad; tuna or chickpea salad on whole-grain crackers; turkey/avocado wrap; tofu stir-fry with brown rice.
Dinner rotation: Baked salmon, quinoa, broccoli; chicken thighs, sweet potato, green beans; bean chili with cornbread; tofu curry with mixed vegetables.
Snacks (protein-forward): string cheese, edamame, protein smoothie, hummus + veggies, peanut butter + apple.
Hydration cues: 8–10 oz water with each meal and med pass; one low-sugar electrolyte drink during heat/illness if advised.
Pantry & Freezer List (Budget-Friendly)
Eggs; canned tuna/salmon; Greek yogurt; cottage cheese; beans/lentils; peanut butter; oats; brown rice; whole-grain pasta; frozen mixed veggies; frozen berries; olive oil; low-sodium soups; chia/flax; low-sugar electrolyte packets.
Everyday Nutrition Tips for Seniors
- Simplify Prep. Batch-cook proteins and grains once weekly. Use single-serve containers to make balanced plates easy to reheat.
- Flavor Wisely. Replace salt with herbs, pepper, lemon, or vinegar to heighten taste and support heart health.
- Snack Strategically. Keep portable protein options—nuts, Greek yogurt cups, or cheese sticks—ready for quick nourishment.
- Mind Medication Timing. Separate iron or calcium from thyroid medication and antibiotics for best absorption.
- Check Labs Yearly. Review B12, vitamin D, iron, and albumin to catch hidden deficiencies early.
- Involve Family or Caregivers. Shared meal prep increases consistency and reduces skipped meals.
Meal Planning Strategies for Caregivers
Caregivers can simplify nutrition tracking by building a “mix-and-match” menu for the week—two proteins, two vegetables, one grain base, and rotating fruit. Use shared phone notes or whiteboards to record hydration and intake. Encourage the senior to choose meals themselves to preserve autonomy.
Overcoming Appetite & Taste Changes
Diminished appetite is common with aging, medication effects, or slower digestion.
- Serve smaller, more frequent meals rather than three large ones.
- Add healthy fats and flavor boosters like olive oil, cheese, or nut butters for calorie density.
- Alternate temperatures and textures—warm soups, chilled fruit, crunchy veggies—to keep meals enjoyable.
These adjustments sustain nutrition without overwhelming the appetite.
Explore the Full Nutrition Series
Protein for Elderly: Essential Daily Requirements & Proven Tips for Seniors (2025 Guide)
Best Protein Powders for Seniors
Hydration Tips for Seniors
Best Electrolyte Drinks / Packets for Seniors (Coming soon)
Constipation in Seniors: A Food-First Plan (Coming soon)
Best Fiber Supplements for Seniors (Coming soon)
Vitamin D & Calcium Basics for Seniors (Coming soon)
Vitamin B12 in Older Adults (Coming soon)
Best Pill Organizers & Automatic Dispensers (Coming soon)
FAQs: Nutrition for Elderly Adults
Q1: How much protein should most older adults eat each day?
≈ 1.0–1.2 g/kg/day, spaced across meals; during rehab or illness 1.2–1.5 g/kg/day with guidance. See Protein Requirements for Seniors (Coming soon).
Q2: What are easy ways to drink enough water without feeling bloated?
Sip 8–10 oz with each meal and med pass; add water-rich foods. Follow clinician targets if fluids are restricted.
Q3: Which vitamins and minerals matter most for seniors?
Vitamin D, calcium, B12, and adequate protein are core priorities. Ask about labs if you have fatigue, falls, or slow healing.
Q4: Do I need a protein shake if I’m eating well?
Food first. Use shakes when appetite is low or targets are hard to reach; choose third-party tested brands with 20–30 g protein/serving.
Q5: How can I increase fiber without gas or discomfort?
Add fiber gradually (+5 g/week) and drink water. Mix ½ soluble + ½ insoluble sources. See Constipation in Seniors: A Food-First Plan (Coming soon).
Q6: What are signs of malnutrition in older adults?
Unintended weight loss, loose clothing, weakness, frequent infections, or poor wound healing. Seek medical review promptly.
Q7: What are the best soft foods for seniors with chewing difficulties?
Scrambled eggs, mashed beans, yogurt, pureed soups, soft-cooked veggies, and smoothies with protein powder provide nutrients safely.
Q8: How does poor nutrition affect recovery after illness or surgery?
Good nutrition shortens recovery time. Protein supports tissue repair; vitamin C, zinc, and vitamin D enhance wound healing; and adequate calories prevent muscle loss. Malnutrition can delay rehab progress, increase infection risk, and extend hospital stays.
Aim for 25–35 g protein per meal, enough fluids, and balanced meals with fruits and vegetables during recovery. If appetite or chewing is limited, nutrient-dense shakes or soft meals like scrambled eggs and soups help fill gaps. Ask your clinician or dietitian about adding a specialized oral nutrition supplement if needed.
Final Thoughts
Start simple: prioritize protein at every meal, carry a water bottle, add a serving of beans or veggies daily, and check vitamin D and B12 with your clinician. Small, consistent habits compound into better strength, fewer falls, faster rehab—and more independence.
A steady foundation of nutrition for elderly adults builds confidence, mobility, and quality of life.
For more on staying mobile and independent, explore our guides on safe home environments and mobility aids.
Continuing Education & Reliable Resources
Staying current with nutrition science helps seniors and caregivers make informed choices.
- The National Institute on Aging offers practical meal and portion guidance for older adults.
- The NIH Office of Dietary Supplements provides evidence-based nutrient fact sheets.
- The USDA MyPlate for Older Adults shows balanced plate visuals adapted for aging.
- The Academy of Nutrition and Dietetics helps you find registered dietitians for personalized care.
Emerging research continues to link nutrient quality with reduced fall risk, cognitive preservation, and faster wound healing—core pillars of mobility and independence.
Medical disclaimer: This content is for educational purposes only and does not replace professional medical advice. Always consult a healthcare provider for personalized recommendations.