Introduction
Pressure ulcers — often called bedsores — are one of the most common and preventable health challenges faced by seniors. They occur when prolonged pressure on the skin cuts off circulation, leading to tissue damage.
For caregivers, learning how to prevent pressure ulcers in seniors is far easier than treating them once they develop. This guide offers practical, easy-to-follow steps you can use daily to protect your loved one’s skin, maintain comfort, and reduce the risk of painful complications.
(For seniors who spend a lot of time in wheelchairs, you may also want to check out our guide to the best wheelchair cushions for added protection.)
What Causes Pressure Ulcers in Seniors?
A pressure ulcer (bedsore) is an injury to the skin and underlying tissue caused by unrelieved pressure, usually over bony areas like the tailbone, heels, elbows, and hips.
- Stage 1: Redness that does not fade after pressure is relieved.
- Stage 2: Blisters or shallow open sores.
- Stage 3: Deep wounds extending into fat tissue.
- Stage 4: Severe wounds affecting muscle, tendon, or bone.
Pressure ulcers affect more than 2.5 million patients in the U.S. each year, creating a major burden on patient outcomes and healthcare costs (NIH).
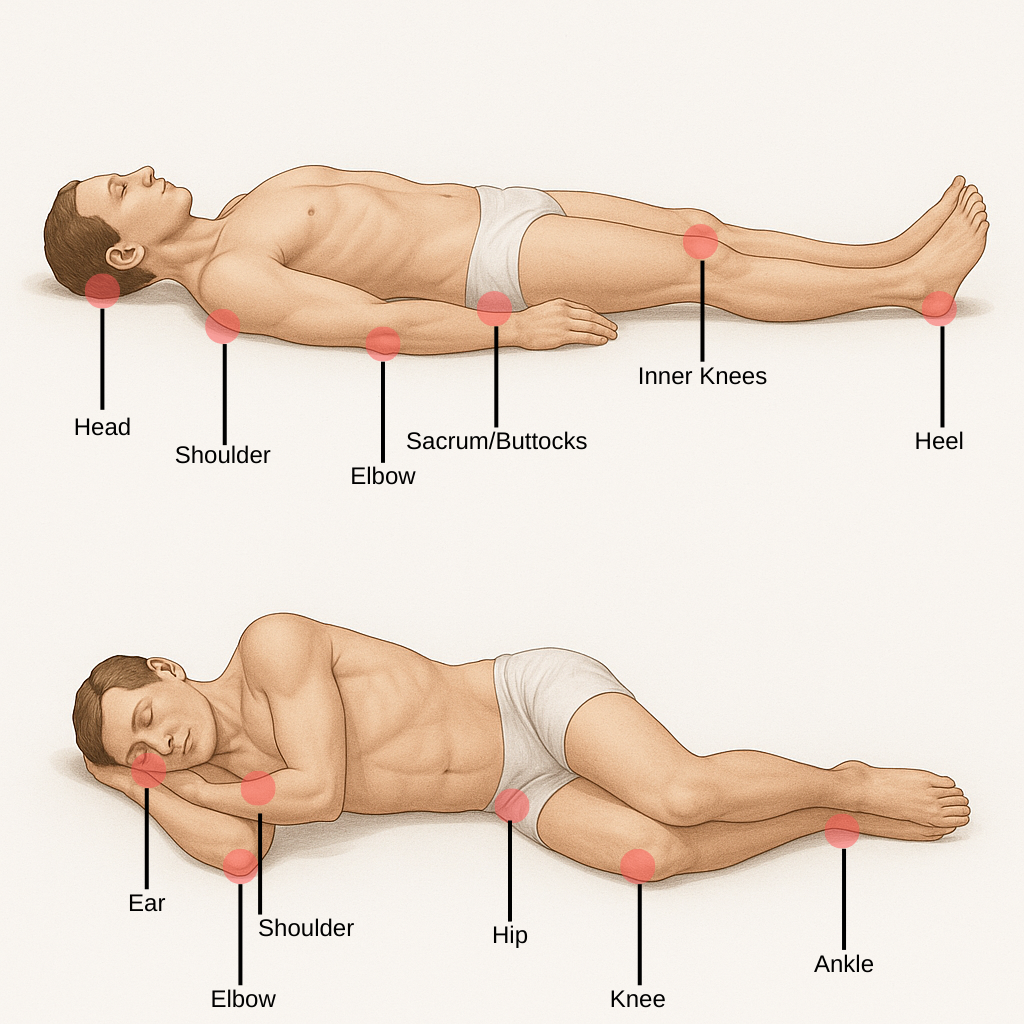
The earlier you catch them, the easier they are to manage — making prevention and daily skin checks essential.
Who Is Most at Risk?
Seniors most at risk of developing pressure ulcers include:
- Bedbound individuals who cannot change position without help, leaving their skin under constant pressure.
- Wheelchair users who sit for long hours, especially without a proper cushion.
- Patients with chronic conditions such as diabetes, circulation problems, or malnutrition that slow healing.
- Seniors with fragile, aging skin or those taking medications like steroids that thin the skin.
(If your loved one uses a walker or rollator to stay mobile, see our guide to the best walkers and rollators for seniors for safer mobility options.)
Proven Strategies to Prevent Pressure Ulcers in Seniors
1. Frequent Repositioning
- Reposition bedbound seniors at least every two hours to reduce constant pressure on the same skin areas.
- Encourage wheelchair users to shift weight every 15–30 minutes, even if it’s just leaning side to side or pushing up with armrests.
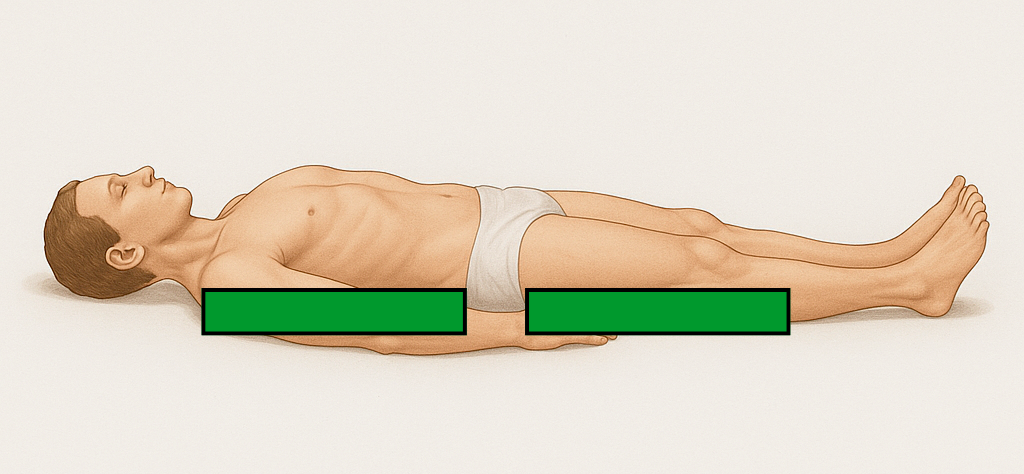
Using Wedges
- Place foam or inflatable wedges behind the back or between the knees to keep seniors in a comfortable side-lying position.
- Wedges reduce the need for constant manual repositioning and help prevent sliding back into pressure-prone positions.
- They improve alignment and comfort, especially for patients who have trouble staying in place after being repositioned.
2. Support Surfaces
- Choose special mattresses or overlays that distribute weight more evenly and lower pressure points.
- Use wheelchair cushions made from gel, foam, or air cells to protect against sores caused by long hours of sitting.
- Investing in proper support surfaces reduces long-term risk and keeps seniors more comfortable.
(Check out our full review of the best wheelchair cushions for practical recommendations.)
3. Skin Care & Inspection
- Perform daily skin checks, especially on bony areas like heels, hips, tailbone, and elbows, to catch early redness.
- Keep skin clean and dry at all times, since moisture increases the chance of breakdown.
- Moisturize daily with fragrance-free lotions to maintain skin elasticity and strength.

Incontinence & Diaper Changing
- Change briefs or bedding immediately after soiling to reduce exposure to moisture, bacteria, and irritants.
- Apply barrier creams with zinc oxide or petroleum jelly after each change to form a protective shield.
- Clean gently with mild, fragrance-free wipes or a soft cloth instead of harsh soaps or alcohol-based wipes that strip natural oils.
- Choose breathable, high-absorbency incontinence products that wick moisture away and keep skin drier for longer.
4. Nutrition & Hydration
- Include protein-rich foods like lean meats, beans, eggs, or dairy to support tissue repair and skin resilience.
- Ensure adequate hydration throughout the day to keep skin supple and less prone to damage.
- Incorporate vitamins and minerals such as vitamin C and zinc to aid healing and strengthen skin health.
5. Mobility & Exercise
- Encourage gentle stretching and range-of-motion exercises to improve circulation and reduce stiffness.
- Assist with transfers to a chair for meals or short sitting periods to promote posture changes and reduce pressure.
- Encourage walking with a walker or rollator for seniors who are cleared to do so, since mobility is one of the best ways to prevent skin breakdown.
⚠️ Important Safety Note: Walking should only be encouraged if a healthcare provider has cleared your loved one for safe mobility. For seniors at high fall risk, focus on safe alternatives like ankle pumps, assisted leg lifts, or supported bed-to-chair transfers.
(See our guide to walkers and rollators for mobility aids that help seniors stay active while reducing risk.)
When to Seek Medical Help
- Contact a healthcare professional right away if redness doesn’t fade after relieving pressure.
- Seek care for blisters, open wounds, or dark patches on the skin, as these can progress quickly.
- Watch for infection signs such as swelling, warmth, pus, or fever, which require immediate attention.
Conclusion
Learning how to prevent pressure ulcers in seniors is one of the most impactful steps caregivers can take to protect health and comfort. Small daily habits — like repositioning, using wedges, maintaining skin care, and encouraging safe mobility — make a major difference.
By combining prevention strategies with the right equipment, caregivers can reduce the risk of painful wounds and help seniors maintain dignity and quality of life.
For related caregiver resources, see:
- Best Wheelchair Cushions for Seniors (2025 Review)
- Best Walkers & Rollators for Seniors (2025 Guide)
- Best Lightweight Wheelchairs for Seniors (2025 Guide)
Disclaimer
This article is for informational purposes only and does not replace professional medical advice. Always consult a healthcare provider before making medical or mobility decisions. Walking or exercise should only be attempted if a physician has cleared your loved one for safe mobility, to avoid falls or injuries.