Intro
If you’ve been feeling more tired than usual, struggling to focus, or noticing tingling in your hands or feet, it might not just be aging — it could be a vitamin B12 deficiency.
Vitamin B12 plays a quiet but powerful role in how your body and brain function. It keeps your red blood cells healthy, supports your nerves, and helps turn food into energy. Yet for many older adults, those B12 levels begin to dip without warning.
Over time, that dip can cause fatigue, balance problems, memory changes, and even mood shifts. The tricky part? These vitamin B12 deficiency symptoms in elderly adults often look like other conditions, so they’re easy to miss.
This guide walks you through what’s really happening, how to catch it early, and what you can do to stay sharp, steady, and energized.
Why Vitamin B12 Matters for Seniors
B12 is one of the body’s hardest-working vitamins. It helps make DNA, keeps nerves insulated so signals travel smoothly, and fuels red blood cell production. Without enough, your cells can’t carry oxygen efficiently, and your nervous system can’t send clear messages.
For older adults, that combination can impact nearly everything — energy, balance, focus, and even wound healing.
Here’s why B12 becomes more important with age:
- Natural absorption declines: The stomach makes less acid and less intrinsic factor (the protein that binds to B12 so your body can absorb it).
- Diet changes: Seniors often eat smaller portions or cut back on meat, dairy, or eggs — all main B12 sources.
- Common medications interfere: Heartburn medicines, diabetes drugs like metformin, and some antibiotics can block absorption.
- Health conditions add risk: Digestive issues, surgery, or autoimmune disorders can make it even harder to get enough B12 from food.
That combination means even healthy eaters can become deficient over time. Understanding how this happens — and how to fix it — is key to long-term health and independence.
The Slow Fade: Recognizing Vitamin B12 Deficiency Symptoms in Elderly Adults

B12 deficiency rarely strikes overnight. It sneaks up gradually, sometimes over years, as the body’s stored supply runs out. Because early signs are subtle, they often go unnoticed until the effects become more serious.
Common Early Symptoms
- Fatigue and weakness: You might feel drained even after sleeping well.
- Shortness of breath or dizziness: The body struggles to deliver enough oxygen to tissues.
- Pale or slightly yellow skin: A sign that red blood cells aren’t forming properly.
- Loss of appetite or weight loss: Low B12 can disrupt digestion and reduce hunger.
Neurological and Sensory Symptoms
- Tingling or numbness in hands and feet: Nerve fibers start to fray without enough B12 to maintain their insulation.
- Balance or walking problems: Seniors may feel unsteady or have trouble climbing stairs.
- Burning sensation in the tongue or mouth: Known as glossitis, it can make food taste different or dull.
- Cold hands or feet: Blood flow and nerve communication slow down.
Cognitive and Emotional Symptoms
- Forgetfulness and “brain fog.” Tasks that once came easily may take extra effort.
- Mood swings, irritability, or depression. Low B12 affects neurotransmitters that regulate mood.
- Confusion or slowed thinking. When nerves in the brain misfire, processing speed drops.
- Difficulty concentrating. You may lose your train of thought more often.
The pattern can look like mild dementia, depression, or even peripheral neuropathy — which is why testing is so important. A simple blood test can confirm whether B12 is the missing link.
Doctor’s Note
“One of the best parts of my job is seeing patients regain their energy and clarity after identifying low B12. Sometimes what feels like aging is really just a fixable nutrient gap.”
— Dr. Jonathan Serman, MD, Wound-Care Physician
Why Deficiency Happens: Common Causes in Older Adults
1. Low Stomach Acid and Intrinsic Factor
Your stomach produces acid and a protein called intrinsic factor. Together, they act like a tag team: acid releases B12 from food, and intrinsic factor carries it into the small intestine for absorption.
As we age, acid levels drop — and without enough intrinsic factor, B12 can’t be absorbed efficiently. Even a diet rich in meat and dairy may not help if absorption fails.
2. Medications That Block Absorption
Certain medications make deficiency more likely:
- Heartburn or acid reflux drugs (like omeprazole or famotidine) lower acid levels.
- Metformin, used for diabetes, can interfere with B12 absorption over time.
- Antibiotics or seizure medicines sometimes alter gut bacteria that help process nutrients.
If you’ve been taking these long-term, regular testing is smart prevention.
3. Digestive Disorders
Conditions such as Crohn’s disease, celiac disease, or a history of intestinal surgery reduce absorption area in the small intestine — where B12 normally enters the bloodstream.
4. Poor Diet or Appetite Changes
Older adults may eat less due to reduced taste, chewing difficulty, or smaller appetites. If meat, eggs, and dairy are limited, it’s easy to fall short of the 2.4 micrograms needed each day.
Digestive changes often go hand-in-hand with low B12 intake. Learn gentle nutrition fixes in our Constipation in Seniors: A Food-First Relief Plan (2025 Guide).
5. Pernicious Anemia
This autoimmune condition destroys the cells that make intrinsic factor. Without it, B12 from food can’t be absorbed at all. People with pernicious anemia usually need lifelong supplements or injections.
6. Alcohol and Chronic Illness
Regular alcohol use or liver disease can deplete stored B12. Since the liver acts as the body’s “B12 bank,” damage there accelerates deficiency.
7. Genetic Factors
Rarely, a hereditary issue prevents B12 from attaching to transport proteins in the blood. These cases are uncommon but remind us that genetics sometimes play a hidden role.
How Vitamin B12 Is Tested and Diagnosed

Testing for vitamin b12 deficiency in elderly adults is straightforward but sometimes overlooked. Ask your doctor to check levels during your next lab work — especially if you have any of the symptoms above.
Common Tests
- Serum B12 level:
- Measures total B12 in the blood.
- Below 200 pg/mL is considered low, though symptoms can appear even at 300 pg/mL.
- Methylmalonic acid (MMA):
- Shows how well your cells are actually using B12.
- High levels mean the vitamin isn’t reaching cells effectively.
- Homocysteine:
- Elevated levels can signal low B12 or folate.
- Complete blood count (CBC):
- Checks for large, fragile red blood cells (a hallmark of B12-related anemia).
If your results are borderline, doctors may repeat testing or check for antibodies linked to pernicious anemia.
More details on these tests can be found on the Mayo Clinic’s Vitamin B12 Anemia page.
Treatment: Getting Levels Back to Normal
Once a deficiency is found, treatment usually works quickly. The goal is to restore levels, rebuild red blood cells, and repair nerve tissue.
1. Oral Supplements
Most people respond well to tablets containing 500–1,000 mcg per day. B12 is water-soluble, so any extra leaves the body through urine — making it very safe. Look for labels that list cyanocobalamin or methylcobalamin as the active ingredient.
2. Sublingual (Under-the-Tongue) Tablets
These dissolve in the mouth and can be easier for those with absorption issues or swallowing difficulty. Studies show they work just as well as standard pills.
3. Injections
For severe deficiency or pernicious anemia, doctors may start with weekly injections for a month, then shift to once a month. This delivers B12 directly into the bloodstream.
4. Nasal Sprays or Gels
Prescription options that avoid both stomach and injections. They’re convenient for maintenance therapy.
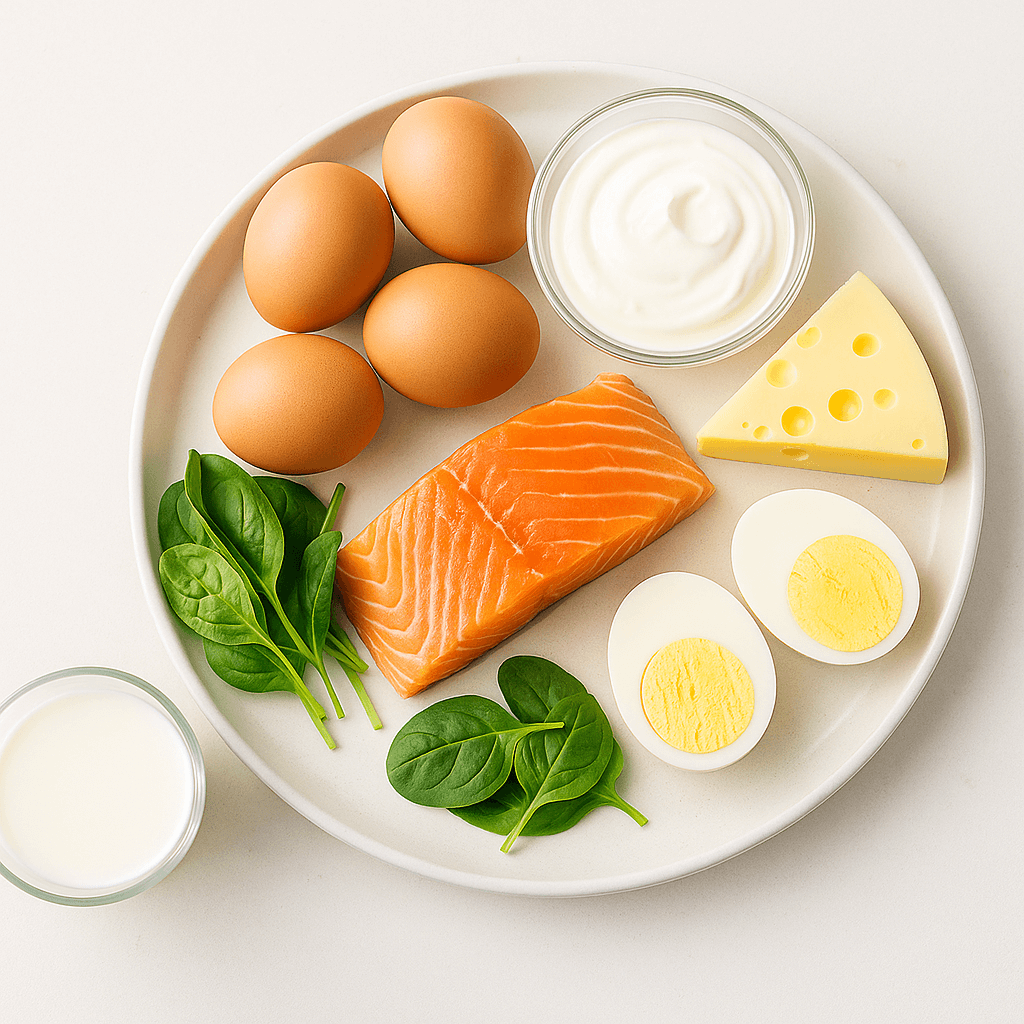
5. Dietary Support
While supplements correct the deficiency, diet helps maintain it. Include:
- Fish and seafood (salmon, tuna, trout, crab, clams).
- Lean meats and poultry (beef, chicken, turkey).
- Eggs and dairy (milk, cheese, yogurt).
- Fortified cereals and plant milks for vegetarians or vegans.
See Harvard Health’s overview of vitamin B12 deficiency for practical diet guidance.
What to Expect During Recovery
Energy often returns within a few weeks once supplementation begins. Memory and concentration improve next, followed by gradual relief of nerve symptoms.
Staying hydrated also supports nerve recovery and energy. See our Best Electrolyte Drinks & Packets for Seniors (2025 Guide) for options that help maintain balance and endurance.
Nerve healing can take several months. If damage has been severe or long-standing, some tingling may persist.
Regular follow-up blood tests every three to six months ensure your levels stay within range. If you have a condition that limits absorption, lifelong maintenance is usually required.
How Much Vitamin B12 Do Seniors Need?
The daily recommendation for adults over 50 is 2.4 micrograms, but that assumes normal absorption. Because the body’s ability to use B12 drops with age, most seniors benefit from 25–100 micrograms per day through supplements or fortified foods.
The body only absorbs what it needs and flushes the rest, so there’s no danger of overdose. Still, extremely high doses aren’t necessary unless prescribed for therapeutic reasons.
Vitamin B12 and the Brain: Protecting Memory and Mood
Low B12 can have surprising effects on mental health.
When levels fall, homocysteine builds up in the blood, which can reduce blood flow to the brain and damage nerve cells. Over time, this may lead to memory problems, confusion, or depression.
Several studies suggest that restoring B12 levels can improve attention, reaction time, and mood — especially in people whose deficiency contributed to cognitive decline.
If you or a loved one has new memory or mood changes, it’s worth asking your doctor to include B12 in the evaluation. It’s a small test with big implications.
Vitamin B12 and Physical Strength
Low B12 doesn’t just affect energy — it can also impact muscles and mobility. Without enough B12:
- Nerves that control muscles fire more slowly, weakening coordination.
- The brain’s communication with the body becomes sluggish.
- Recovery from illness, wounds, or surgery can slow down because cells don’t regenerate efficiently.
Adequate B12 supports balance, reduces fall risk, and promotes wound healing — key goals for staying mobile and independent. For added muscle support, see Best Protein Powders for Seniors (2025 Guide).
Prevention: Staying Ahead of Deficiency
You can prevent B12 deficiency before it starts. Here’s how:
- Ask for annual screening once you’re over 60 or if you take acid blockers or metformin.
- Eat B12-rich foods daily. Seafood, eggs, and dairy are simple, reliable options.
- Use fortified foods or supplements if you’re vegetarian or have low appetite.
- Limit alcohol to protect stomach and liver health.
- Manage gut issues early. Treat reflux, gastritis, or bowel conditions promptly.
- Keep your overall nutrition balanced. Vitamins B6, folate, and iron work alongside B12 in blood and nerve health.
For a broader look at nutrition strategies, see Nutrition for Elderly: 2025 Guide to Healthy Aging & Mobility Support.
When to Seek Medical Care
Call your healthcare provider if you experience:
- Persistent tingling or numbness in your feet or hands
- Frequent stumbling, dizziness, or balance loss
- Ongoing fatigue even after rest
- Sudden memory lapses or mood changes
- Pale or yellowish skin, or a sore tongue
Early treatment can prevent permanent nerve damage and bring major improvements in quality of life.
The Cleveland Clinic’s guide to B12 deficiency anemia explains what to expect during evaluation and recovery.
Frequently Asked Questions
1. What are the warning signs of vitamin B12 deficiency in older adults?
Fatigue, numbness or tingling, balance problems, and memory changes are common. Many also experience mood swings or pale skin. Symptoms can progress slowly, so don’t ignore subtle changes.
2. How do doctors diagnose B12 deficiency?
Through blood tests that measure B12, methylmalonic acid (MMA), and homocysteine. If your B12 is borderline, additional tests may check for absorption problems.
3. What causes low B12 in seniors?
Reduced stomach acid, certain medications, digestive disorders, and autoimmune disease are main culprits. Diet and alcohol use can also play a role.
4. Can low B12 cause dementia or depression?
Yes. Low B12 interferes with brain chemicals that control mood and memory. Restoring levels often improves alertness and energy, though it doesn’t reverse other causes of dementia.
5. How long does recovery take?
Energy returns in a few weeks; nerve symptoms may take several months. Maintenance therapy prevents relapse.
6. Do vegetarians and vegans need B12 supplements?
Absolutely. Since plant foods contain little or no B12, fortified cereals, plant milks, or supplements are essential.
7. Is B12 safe to take daily?
Yes. Because it’s water-soluble, the body flushes out excess. Side effects are rare.
8. What’s the difference between methylcobalamin and cyanocobalamin?
Both work well. Methylcobalamin is the natural form used in the body; cyanocobalamin is more common and affordable. Either can restore levels effectively.
9. How often should seniors get tested?
Once a year, or sooner if new symptoms develop or medications change.
10. Can B12 deficiency affect wound healing?
Yes — cells need B12 to repair tissue. Deficiency can slow healing after surgery or injuries, which is why maintaining good levels is crucial.
Final Thoughts
Vitamin B12 deficiency symptoms in elderly adults are more than just a minor nutritional issue — they can affect memory, mobility, and independence. The good news is that deficiency is both preventable and reversible.
Regular testing, balanced eating, and consistent supplementation can restore vitality and protect long-term health. Even small changes — like adding fortified foods or asking for a B12 check at your annual visit — can make a noticeable difference in energy and focus.
To strengthen your bones and overall mobility alongside healthy B12 levels, read Bone Health for Seniors: Vitamin D & Calcium Basics (2025 Guide) — part of our Nutrition for Elderly series at Mobility With Ease.
Disclaimer
This content is for educational purposes only and should not replace professional medical advice. Always consult your healthcare provider before making changes to your diet, supplements, or medications.